Onychorrhexis (ICD code L 60.3) is a type of dystrophy of the nail plate in which it splits along the direction from the free edge to the growth zone. Occurs in women and men. Depending on the cause, onychorrhexis is observed only on one nail or on all of them at once. Cracks can be single or multiple, of different lengths and depths.
What causes?
The causes of onychorrhexis are divided into internal and external. When the body weakens, chronic pathologies, infections, the nail initially grows fragile. It cracks easily, delaminates, breaks off from the free edge. Due to impaired blood flow and chronic diseases, longitudinal splitting of the nail is often found in older people. The older the person, the higher the risks. Aging of the body is the most common reason.
Internal factors include:
- diabetes, thyrotoxicosis, cause metabolic disorders;
- atherosclerosis, lead to a decrease in the lumen of blood vessels, a decrease in blood flow, and the supply of nutrients;
- eczema, psoriasis, cause inflammation, disruption of the nail structure;
- autoimmune diseases (Raynaud's syndrome, vasculitis), damage the walls of blood vessels, nutrition of the matrix, reduce the strength of the resulting plate;
- lack of vitamins and minerals in the body due to malnutrition, eating disorders (anorexia, bulimia) or gastrointestinal diseases that interfere with the absorption of nutrients and change the chemical composition of the plate;
- fungal infection, provokes an inflammatory process, destroys the healthy structure of the nail;
- tumor diseases.
External factors can cause dystrophy:
- injuries received during a manicure or pedicure;
- household damage;
- working with cleaning agents and detergents without protective gloves;
- wearing shoes that don't fit;
- features of the profession: working at a computer with nails tapping on the keyboard, or playing the piano;
- continuous wearing of gel polish or artificial coverings;
- using acetone-based nail polish removers;
- habit of biting nails;
- frequent contact with water, alcohol, solvents, chemicals that dry out and damage the plate;
- Excessive length, improper cutting of nails.
In children, onychorrhexis is caused by trauma, decreased immunity, and previous infectious diseases.
Skin diseases
When answering the question of why the skin under the nails cracks, it is also necessary to mention skin diseases. Such ailments may be non-infectious or infectious in nature. In the first case, a person develops psoriasis or eczema. As for infectious diseases, this includes fungal infections. Skin diseases provoke the formation of deep cracks under the nails, around them, between the fingers, and also on the palms.

What are the symptoms?
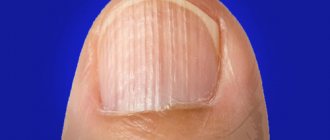
The main sign is the presence of longitudinal cracks on the plate, running from the free edge to the center or base of the nail. They look like grooves or furrows. Depending on the cause, there may be one or several cracks, only on one finger or more. Onychorrhexis affects the fingernails and toenails, but is more common on the hands. On the feet, only the big toe is predominantly affected.
What onychorrhexis looks like is shown in the photo of the nail below:
In addition to longitudinal cracks, thinning of the plate, a change in color to yellowish or grayish, and an uneven laminated free edge are also possible. Due to increased fragility, longitudinal splitting is often combined with transverse splitting, which is called onychoschisis.
Vertical grooves on the nails, reminiscent of onychorrhexis, are characteristic of trachyonychia. And their treatment principles are similar. This is a type of onychodystrophy in which the nails become dull, rough, and covered with grooves and scales.
White spots on the outside of the nail plate
They look like white dents less than a millimeter in diameter. Typically, such spots on the nails are found in people suffering from psoriasis, a skin disease in which the skin becomes very flaky.
White spots on the nails also occur in people with sarcoidosis, pemphigus, and alopecia areata. Such point changes in the nail plate can also occur when it is mechanically damaged.
White spots on the nails are the result of microdamage to the nail plate, and not, as many believe, a deficiency of vitamin C.
Diagnostics
If you find a plate splitting, contact a podiatrist or dermatologist to prevent the condition from getting worse. If left untreated, the crack will grow and reach the free edge. It will divide the nail into two halves and cause detachment from the bed. In addition, violation of the integrity of the plate opens access to pathogenic pathogens and often leads to bacterial or fungal infectious complications.
The specialist will examine the structure of the plate, assess the severity of the damage, suggest how to treat onychorrhexis of the fingernails or toenails, and how to improve their appearance.
To find out the cause, he will ask the patient about chronic diseases and prescribe additional examinations:
- examination of a nail scraping for fungus;
- general blood test, sugar test;
- consultation with an endocrinologist, gastroenterologist, vascular surgeon;
- microscopic examination;
- examination with a dermatoscope at 10x magnification.
Treatment methods for hyperkeratosis of the nail plate
Hyperkeratosis is treated by a highly specialized specialist – a podiatrist. Therapy combines systemic and local methods and is prescribed after a comprehensive diagnosis. This approach allows you to accurately influence the cause of the pathology, reduce treatment time, and avoid complications and relapses. Since in most cases, subungual hyperkeratosis develops against the background of nail fungus, the patient is prescribed antifungal drugs - tablets, varnishes and ointments.
Local antifungal treatment and medical pedicure
Local treatment is aimed at suppressing fungal microflora and reducing keratinization. To do this, the clinic performs a medical pedicure - the surface layers of the thickened nail are removed with a cutter.
Baths
It is recommended to take warm salt foot baths every day - dissolve 100 grams of sea salt in 10 liters of water. After the procedure, the steamed tissues of the surface of the nail and the skin around it are removed with pumice and buffs. Then the local drug prescribed by the doctor is applied.
Removing the nail plate
In advanced cases, in order to ensure the delivery of drugs to the affected tissues, complete removal of the nail plate is indicated using mechanical cutters, special compounds and patches.
Diet
To get rid of the fungus, it is recommended to adjust your diet. Sweets and yeast baked goods are excluded from the menu. The diet is balanced in proteins, fats, carbohydrates, vitamins and microelements under the supervision of a nutritionist.
Hygiene
Fungal infections actively multiply in a warm, humid environment, so the inner surface of shoes is treated daily with a pharmaceutical disinfectant solution, and socks, tights and stockings are washed daily. Shoes are changed if necessary - they should not stimulate foot sweating. Scissors and nail files must be strictly individual and treated with a disinfectant solution after use. You will also have to temporarily avoid going to saunas and swimming pools to prevent contact infection.
Traditional methods
Fungi are not sensitive or slightly sensitive to nonspecific agents, therefore traditional methods of treating nail hyperkeratosis are ineffective. Under their influence, the fungal flora develops immunity and infects new structures. The disease becomes severe. Podologists strongly recommend that if you suspect nail hyperkeratosis, you should immediately contact a specialist.
It is impossible to restore a nail plate affected by hyperkeratosis; you can cure the disease and wait until a healthy nail grows. The course of therapy is from 2 to 6 months. After 2 weeks and 2 months after complete elimination of symptoms, control tests are taken to determine the presence/absence of fungus.
How to treat?
To treat onychorrhexis, an integrated approach is used, aimed at eliminating the cause, normalizing metabolic processes, and strengthening the structure of the nails. If these conditions are met, treatment gives a good result. True, it takes up to six months, since the nail plate grows slowly, on average by 1 mm per week. The matrix where nails are formed is hidden under the skin of the lower roller, at a distance of 4 mm from the cuticle. It will take 4 weeks just to improve his condition, and to change the plate on his fingers it will take 4 to 6 months.
Treatment is selected depending on the severity of the injuries and the person’s health status. When identifying concomitant pathologies that cause longitudinal clefting, attention is paid to their treatment.
To strengthen nails the following is prescribed:
- massage;
- vitamins, amino acids, minerals;
- medicinal baths;
- drugs to strengthen the walls of blood vessels and improve blood circulation in the extremities;
- physiotherapy (paraffin therapy, ozokerite, mud masks).
Traditional methods and remedies for the treatment of onychorrhexis of nails include masks or baths with natural oils, oil solutions of vitamins, gelatin, as well as moisturizing and nourishing creams. They help strengthen nails and accelerate regeneration processes. But it is better to discuss the safety of their use with your doctor.
In case of deep, long cracks, the plate is reinforced with artificial materials to stabilize it.
Primary measures for nail injury
Help for the victim must be provided as quickly as possible. The result of treatment and the speed of recovery will depend on its timeliness.
Necessary:
- remove all jewelry from fingers;
- stop bleeding if it occurs: place the wounded finger under cold water;
- moisten a piece of clean cloth, a cotton pad, a bandage with chlorhexidine or a solution of hydrogen peroxide and press it to the wound;
- if possible, apply ice to the injured finger - this will prevent swelling from developing and will calm the pain;
- to reduce pain, the injured limb is held above the level of the heart;
- after the bleeding has stopped, disinfection is carried out using iodine (only the edges of the wound are treated);
- if swelling appears, you can apply an iodine mesh to your finger;
- if the pain does not subside, you should take analgin or ibuprofen;
- Apply a sterile bandage to the wound.
Care and prevention
When treating onychorrhexis, as well as for its prevention in the future, it is important to properly care for the nails, skin of the hands and feet.
What rules must be followed?
- Wash dishes and use any cleaning agents or detergents only with gloves.
- For manicure, choose high-quality varnishes with a harmless composition; do not use removers containing acetone to remove nail polish.
- Avoid frequent contact with water.
- When treating onychorrhexis, it is not recommended to do a manicure or apply any coatings to the nails other than those prescribed by the doctor. In the future, take breaks from wearing gel polish and artificial nails.
- Take care of your drinking regime and a nutritious diet, including fruits, vegetables, and low-fat protein foods.
- Do not grow your nails too long; periodically get medical manicures and pedicures at podiatry centers.
- Massage your hands and feet daily, moisturize the skin on your arms and legs with nourishing creams.
As a rule, onychorrhexis does not cause pain or inflammation, but you still need to go to a podiatrist with this problem. The specialist will prescribe the correct treatment, which will speed up the recovery of the nail and prevent the development of complications. He will also tell you about the rules of care at home so that splitting or splitting of nails no longer bothers you.
13 1
Temperature
When considering the reasons for the appearance of such a symptom, sudden changes in temperature should also be included here. The fact is that sensitive skin reacts to frost and cold. The skin becomes dry, cracks form around the nails, as well as under them. If you do not take any measures, the wounds will become deeper and larger. They hurt a lot and cause discomfort to their owner, so during the cold season it is necessary to pay special attention to the hands.