05/24/2018 Many people who discover a spot under their nail begin to search on the Internet to find out what it could be? And it turns out that this can be a fatal disease - subungual melanoma.
In this article we will look at:
- concept of subungual melanoma;
- the chances of this type of tumor occurring;
- photos of symptoms with histological confirmation;
- ways to distinguish subungual melanoma from hematoma;
- procedures to clarify the diagnosis;
- prognosis and treatment.
Subungual melanoma – what is it?
The share of melanoma among skin tumors is only 4%. But it is from this malignant neoplasm that 80% of patients with skin tumors die [1]. In Russia, about 8,717 people a year currently develop skin melanoma (data for 2012) [2]. Subungual melanoma is located in the nail bed and usually appears as a stripe on the nail.
Sign up for the webinar “Carcinogens in cosmetics: truth, lies and... marketing”
Main factors: what causes longitudinal ones?
Physiological reasons
- Presence of age-related changes.
- Improperly organized nutrition.
- Damage to the base of the nail plate due to improperly performed manicure.
- Dehydration of the body.
Diseases

- Nail fungus.
- Cardiovascular diseases.
- Damage to the central nervous system.
- Arthritis.
- Gout.
- Infectious diseases.
- Functional disorder of the digestive or endocrine systems.
- Avitaminosis.
- Low hemoglobin level.
- General intoxication of the body due to bad habits.
- Diabetes.
- Spinal diseases.
- Metabolic disease.
What are the chances of this type of tumor occurring in a resident of Russia?
Of the total number of melanomas, the share of this tumor is only 2% [3], i.e., in absolute values, in 170 people per year. Against the background of the country's total population of 146,000,000, this, in my opinion, is very small. At the same time, a low incidence rate does not eliminate the possibility of getting sick.
For representatives of other skin phototypes other than 2, the chances may be very different. Representatives of the Mongoloid and Negroid races have a higher (up to 40%) chance of developing melanoma of the nail bed [4, 5].
Where does subungual melanoma appear most often?
The tumor most often affects the big toes [3].
What does subungual melanoma look like? Photos and signs.
All pictures below are histologically confirmed and not taken from the Internet. The source is indicated in square brackets. There are 2 most common signs:
Sign I
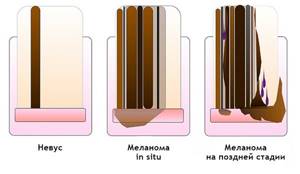
Most often, subungual melanoma appears as a brown or black stripe. The strip starts from the nail fold and ends at the edge of the nail. This condition is called longitudinal melanonychia. Some medications can cause such bands to appear - retinoids and Docetaxel (Taxotere) [10]. This sign can also occur in conditions not associated with melanoma, for example, with fungal infection of the nail, pigmented nevus of the nail bed.

Subungual pigmented nevus in a 13-year-old boy [9]
Subungual melanoma stage I, 0.2 mm according to Breslow [10]
Sign II
The most common sign of this type of melanoma is Hutchinson's sign - a transition of pigmentation to the nail fold or fingertip. This feature is visible in 7 of the 8 images below. At the same time, it cannot be stated unequivocally that this symptom occurs only with melanoma. It can also be observed with a transparent cuticle [10].

8 cases of subungual melanomas in situ (initial stage) [6]

Subungual melanoma of the thumb with level 4 invasion according to Clark, thickness according to Breslow is not specified [8]

Subungual melanoma, Breslow thickness 1.5 mm [7]
Prevention
Complicated and sometimes unpleasant treatment will not be necessary if you follow the following preventive measures:

- Make sure that your diet is rational, balanced and organized in accordance with the characteristics of your body.
- Give up bad habits and too intense physical activity.
- Be careful and follow safety precautions when working with heavy tools.
- Take precautions when visiting the bathhouse and swimming pool, and choose your manicurist carefully.
Be carefull! Carefully monitor the condition of your nails. Perhaps this will help you identify health problems in time and get rid of them.
How to distinguish subungual melanoma from everything else?
Here is a fairly simple algorithm.

Algorithm for the differential diagnosis of benign melanonychia and the same condition in melanoma [8]
ABCDEF rule for diagnosing nail bed melanoma
And (age) age - the peak incidence of subungual melanoma occurs between the ages of 50 and 70 years, and also denotes races with an increased risk: Asians, Africans - they account for 1/3 of all melanoma cases.
B (brown to black) – the color is brown and black, with a stripe width of more than 3 mm and blurry boundaries.
C (change) – change in the color of the nail plate or no change after treatment. D (digit) – finger as the most common site of injury.
E (extension) - spread of pigmentation to the nail fold or fingertip (Hutchinson's symptom).
F (Family) – relatives or the patient have a history of melanoma or dysplastic nevus syndrome. [eleven]
How to distinguish a hematoma from a subungual melanoma by dermatoscopy

Hematoma: [10]
- It moves under the nail along with its growth. You can track this by taking a photo of the formation against the background of a ruler located longitudinally. It is important to note that a hematoma does not always appear due to trauma.
- Color from red-blue to black-blue.
- Does not transfer to the cuticle, nail fold and fingertip.
- Does not involve the entire nail in the longitudinal direction.
- May change within a few weeks.
- The color intensity decreases from the center to the periphery.
- It may be preceded by trauma.
- Small blood spots oriented towards the edge of the nail on dermatoscopy
Subungual melanoma: [12]
- Heterogeneous color, irregular stripes with melanonychia.
- Triangular stripes.
- Spreads on the nail plate, free edge of the nail or fingertip.
- Destruction or dystrophy of the nail.
Treatment of stripes on nails

Getting rid of grooves is aimed at eliminating the cause that provoked this symptom. Complex therapy will help restore the attractiveness of your nails:
- If a fungus is detected, local and systemic antifungal drugs are prescribed. They help destroy spores and mycelium of pathogenic microorganisms. Among the popular drugs are Ketoconazole and Terbinafine.
- When diagnosing problems with the liver, the organ is cleansed with a diet and biological supplements that support the diseased organ. Additionally, multivitamin complexes Gerimax Energy and Angiovit are prescribed.
- For diseases of the nervous system, sedatives are prescribed: Valerian, Motherwort. Additionally, the patient is recommended to take walks and adhere to a rest regime.
Diet
The health of your nails directly depends on a proper diet. If stripes and other defects appear on them, it is necessary to exclude fast food, easily digestible carbohydrates (baked goods, sweets), carbonated drinks, alcohol, highly salted or spicy foods from the daily menu. Water regime is also important - you need to drink at least 1.5 liters of plain water per day. Healthy foods:
- rabbit meat, poultry (iron);
- red fruits: apples, pomegranates, currants (manganese, vitamins C, B, E)
- black radish (retinol, glycosides);
- dried apricots, nuts, sesame (calcium);
- fish oil (vitamin D);
- oysters, wheat bran (zinc);
- leafy vegetables, beans, lentils (magnesium);
- brown rice, oatmeal (silicon);
- herring, mackerel, squid (selenium).
Care
During treatment of the nail plate, special care is needed. It includes a home manicure at least once every 14 days, regularly lubricating the nails with a moisturizer, and cleansing the nails with a gentle peeling. Traditional recipes used at home will also help strengthen:
- Rub a mixture of vitamins A and E in oil into the cuticles and nail growth area daily. It is better to do the procedure at night until the condition improves. Rubbing will help saturate them with the necessary vitamins.
- Soak a cotton swab in apple cider vinegar and apply to the affected nails. Secure the top with a band-aid, put on cotton socks or gloves and go to bed. In the morning, wash the treated areas with laundry soap. Do the procedures 2 times a week until the problem goes away. Vinegar will help get rid of infection and strengthen the nail plate.
- Make hand baths using vegetable oils (jojoba, almond, sea buckthorn, olive, linseed). Warm it until warm and soak the affected nails for 10 minutes. After the procedure, blot the oil with a napkin and wash your hands (feet) with soap. First do a daily course of 10 procedures, then once a week for preventive purposes. Vegetable oils will improve the structure of the nail in a short time.

Bibliography
- Miller AJ, Mihm MC. Melanoma. N Engl J Med. 2006; 355:51-65.
- Data from the Globocan 2012 study, International Agency for Research on Cancer (IARC): https://gco.iarc.fr/today/online-analysis-multi-bars?mode=cancer&mode_population=hdi&population=643&sex=0&cancer=29&type=0&statistic=0&prevalence= 0&color_palette=default
- Kuchelmeister C, Schaumburg-Lever G, Garbe C. Acral cutaneous melanoma in caucasians: clinical features, histopathology and prognosis in 112 patients // J. Dermatol. – 2000
- Takematsu H, Obata M, Tomita Y. Subungual melanoma. A clinicopathologic study of 16 Japanese cases // Cancer. – 1985
- Wu XC, Eide MJ, King J. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States, 1999–2006 // J. Am. Acad. Dermatol. – 2011.
- Jae Ho Lee, Ji-Hye Park, Jong Hee Lee, Dong-Youn Lee. Early Detection of Subungual Melanoma In Situ: Proposal of ABCD Strategy in Clinical Practice Based on Case Series Ann Dermatol. Feb 2022; 30(1): 36–40.
- Stephan Braun, MD and Peter Gerber, MD. Subungual malignant melanoma. CMAJ. 2015 Sep 8; 187(12): 909.
- Pierre Halteh, Richard Scher, MD, FACP, Amanda Artis, MS, MPH, and Shari R. Lipner, MD, PhD. A Survey Based Study of Management of Longitudinal Melanonychia Amongst Attending and Resident Dermatologists. J Am Acad Dermatol. May 2022; 76(5): 994–996.
- Kamran Khan and Arun A Mavanur. Longitudinal melanonychia. BMJ Case Rep. 2015; 2015: bcr2015213459.
- Holger A. Haenssle, Andreas Blum, Rainer Hofmann-Wellenhof, Juergen Kreusch, Wilhelm Stolz, Giuseppe Argenziano, Iris Zalaudek, and Franziska Brehmer. When all you have is a dermatoscope— start looking at the nails. Dermatol Pract Concept. 2014 Oct; 4(4): 11–20.
- Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol. 2000 Feb;42(2 Pt 1):269-74.
- Haenssle HA, Brehmer F, Zalaudek I, Hofmann-Wellenhof R, Kreusch J, Stolz W, Argenziano G, Blum A. Dermoscopy of nails. Hautarzt. 2014 Apr;65(4):301-11. doi: 10.1007/s00105-013-2707-x.











